What is an ACL injury?
An ACL injury is a serious injury that occurs to many athletes involved in rigorous or competitive sports.
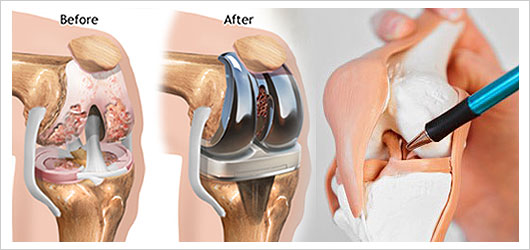
The anterior cruciate ligament or ACL is a band of fibrous tissue or ligaments that connect the thigh bone to the shin.
This part of the knee helps ensure people do not end up rotating or twisting their knees uncontrollably.
ACL injuries are very common among athletes, especially those who are engaged in sports that involve rigorous jumping, pivoting, running, and sudden stops.
Torn ACL will require proper rehabilitation to ensure full recovery.
This type of injury should not be taken lightly as sans proper treatment and medical attention, it can leave the individual in extreme pain.
If you are involved in rigorous sports, the tendency of this type of injury occurring is relatively high.
For those who are involved in challenging sports and those who are experiencing this kind of injury, the following self-management (and prevention) tips can come in handy.
What needs to be done in the first 24 hours?

The first 24 hours after an ACL injury, affected individuals will experience extreme pain.
Inflammation will also manifest.
These symptoms are usually evident the first 2 hours after the injury occurred.
For proper treatment and self-management, the R.I.C.E. method is considered ideal:
Rest – resting the injured area should be a priority. Make sure you do not submit the affected area to further stress and strain so complications will not occur.
Ice – putting ice on the area every 2 hours (20 mins each time) is also recommended.
Compression – ideally, the injured area should be wrapped in elastic bandage.
Elevation – elevating the knee when laying down is also advisable. You can make use of pillows or other mechanical device for this purpose.
Seeing a sports doctor or a therapist for further and thorough evaluation should be done after administering first aid treatment.
How do you help ensure ACL injuries are prevented?
Regardless if you are involved in competitive/extreme sports or in a job that puts you at risk for ACL injuries, knowing the necessary prevention tips should be considered imperative.
Fortunately, for starters, there are proper training guides and exercises that can help significantly decrease the chances of an ACL injury occurring.
Once you have completed the assessment, you can visit your trainer, physical therapist, or doctors specializing in sports injuries so they can provide you with instructions, feedback, and insights you can integrate in your training and activities.
Some programs can include:
Exercises that help strengthen the abdomen, pelvis, hips, and the core.
Exercises that will not only strengthen but also stabilize the muscles. This also include exercises that provide balance.
Proper training techniques on the proper running, jumping, and landing should also be taught.
Proper training techniques on the right style of cutting, rotating, and landing should also be taught.
Proper management and treatment of ACL injuries is done on a case to case basis. To get the best treatment intervention, visit www.bjios.sg right away.