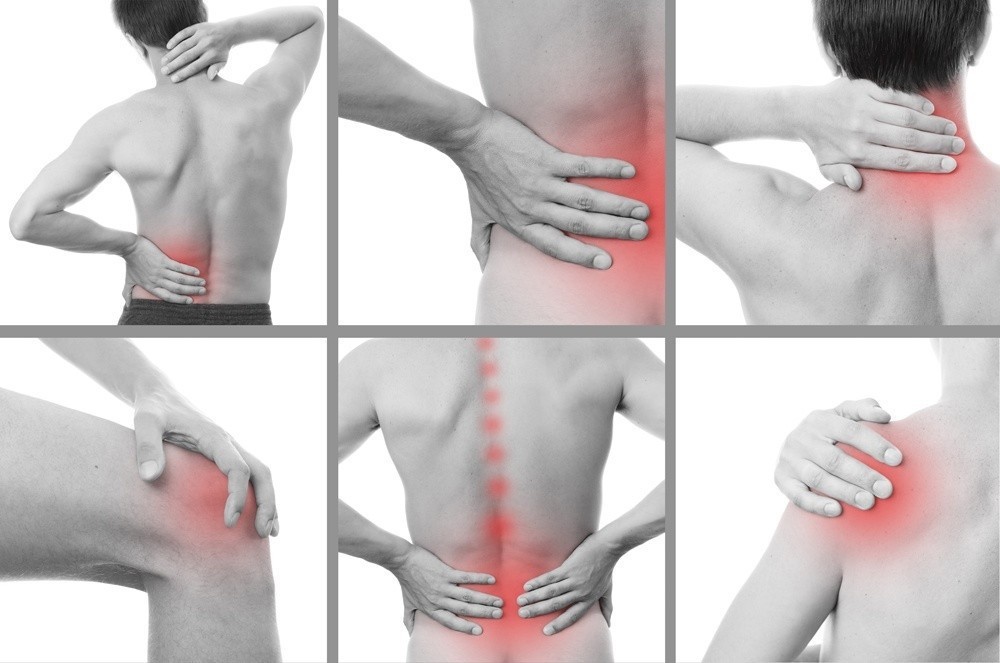
The significance of our joints cannot be overstated.
Aside from helping us move and providing us with the much needed support, the joints also form the connections between the bones of the body.
Joint pain brought about by injury or disease will not only result to a lot of pain but will most likely also impede your movements.
Joint pain can be a result of a lot of conditions—gout, rheumatoid arthritis, sprains, osteoarthritis, and strains to name a few.
Joint pain can also be debilitating or just mildly irritating.
Acute joint pains usually disappear after a few weeks.
Chronic joint pains on the other hand can linger for several months.
Whatever the case may be, what is certain is that joint pain can definitely impact your quality of life.
Prevention
Spare yourself from the inconvenience and aches joint pain can bring by taking to heart the following tips:
Get rid of the excess pounds
You may not be aware of it but the more obese or overweight you are, the more strain you are likely to put on your hips, knees, and back.
If you have been finding it hard to keep the excess pounds off, you might want to consider getting professional help.
Your doctor will be able to provide guidance and recommend programs you can try to safely and effectively get rid of the extra pounds.
If anything, find motivation in the fact that losing even just a pound can take as much as four pounds of pressure from your knees.
That should get you off to a good start if you want to get rid of joint pain once and for all.
Exercise and stay active

This golden rule will do you a whole lot of good especially if you want to keep joint pain at bay.
The more you exercise and stay active, the lesser you’ll experience stiffness and joint pain.
Also, show your joints some love by changing positions every now and then while you are reading, working, or watching your favorite shows on TV.
Ensure you also leave your desk every once in a while so you’d be able to move and effectively keep stiffness at bay.
Do only low-impact exercises
If you want to stay fit but you want to take good care of your joints at the same time, opting for low-impact exercises is the best way to go.
Thankfully, there’s no limit to the number of low-impact exercises available at your disposal.
Joint friendly exercises you can consider include bicycling, walking, strength training, and swimming.
Treatment
For those who are already suffering from joint pain, it is reassuring to know that there are plenty of effective treatment options available at their disposal.
Some of the treatment options include:
Medications
If you have joint pain that ranges from moderate to severe (coupled with swelling), over-the-counter or prescription non-steroidal anti-inflammatory drugs are the likely option.
Aspirin, ibuprofen, and naproxen sodium are some of the likely medications that will be prescribed.
However, if you experience mild pain sans swelling, acetaminophen would be given.
If your joint pain is severe, your doctor may prescribe a strong opioid medication.
However, since opioids can cause drowsiness, it should only be taken upon the doctor’s recommendation.
Topical Agents
When it comes to relieving joint pain brought about by arthritis (or other conditions), capsaicin has been proven effective.
While it can sometimes cause burning or stinging, it has no other known side effect.
Injections
If oral and topical medications won’t provide the much needed relief, a steroid medication injected directly in the joints might be recommended.
The injection is administered every three to four months.
Steroid injections are often the treatment recourse for patients suffering from arthritis, tendinitis, and other joint diseases.
Physical Therapy
Your physical therapist can help effectively strengthen your muscles, stabilize your joint, and improve your motion range.
They also make use of various techniques like ultrasound, electrical nerve stimulation, and cold or heat therapy to provide the much needed relief.
Joint pain keeping you down and hindering you from enjoying a pain-free existence? Let the experts at www.bjios.sg help you out.