An ACL injury or a torn anterior cruciate ligament injury is considered one of the most common (not to mention one of the most painful) injuries anyone can have.
The injury often occurs in individuals who are engaged in sports that entail frequent jumping or running, causing stress and strain to the ligament.
This type of injury is often considered one of the most painful because it involves the knees, one of the parts of the body that has the most nerves.
What is the ACL?
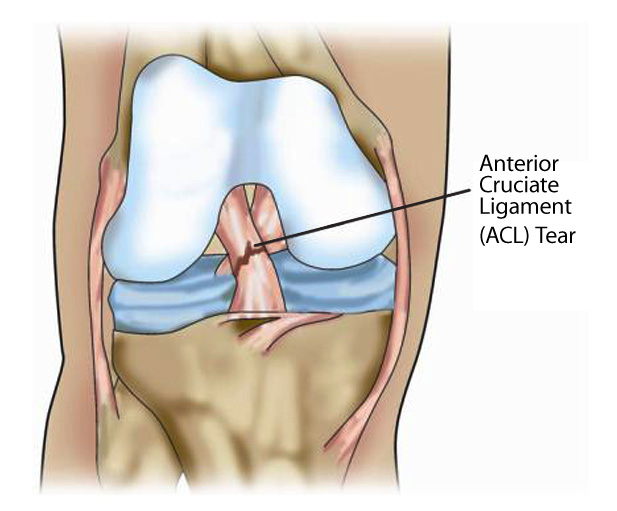
The anterior cruciate ligament or ACL is one of the four major ligaments found in the knee.
It is located in the knee’s middle and it prevents the shin bone from sliding in the front of the thigh bone.
The four ligaments situated in the knees provide the stability the knees need in order to work properly.
When forced or extended beyond their capabilities, these ligaments will be subjected to stress and strain and might tear or rupture.
What are the common symptoms of an ACL injury?
Typically, a torn ACL has 4 common symptoms.
It must be noted that this type of injury may require both surgery and prompt rehabilitation.
The most typical symptoms include:
- A pop or a popping sound during the injury. This popping or pop is often very distinct.
- An onset of intense pain. The pain associated with ACL injuries are often described as searing or burning.
- The first few hours after the injury, intense swelling might manifest around the area that is injured.
- Straightening or bending the knee might cause tightness and pain. Attempting to move the knee in any direction may also result to excruciating pain.
There are certain injuries however that will manifest some of the same symptoms of an ACL injury.
Some of these conditions or injuries include bone breakage, injuries to the knee cushions, and injuries to other parts of the knee like the ligaments.

What is chronic ACL deficiency?
The condition occurs when the joints of the knee becomes chronically unstable.
When this happens, the knees would give in to the pressure and give out.
Pain and inflammation may also manifest and movement will become very uncomfortable and challenging.
While not all who has an ACL injury might develop this deficiency, those who have had a history have a higher chance of developing the condition.
In cases where ACL injuries evolve into recurrent and lifelong ACL deficiency, the affected individual will experience inflammation and pain in the affected area especially when the knee gives out or buckles.
To increase your chances of keeping ACL deficiency at bay, it is important to ensure proper rehabilitation and restored function is observed prior to commencing with the performance of routine activities.
Sans thorough rehabilitation and restored function, an ACL deficiency has a huge chance of occurring.
Eventually, some cases of ACL deficiency can lead to osteoarthritis—another condition that affects the joints and the bones. To know more about osteoarthritis, click here.
While ACL injuries can be prevented, it is sometimes inevitable especially in people involved in rigorous sports.
To prevent any complications, it is important to check with your doctor right away so proper treatment and rehabilitation can be administered. Visit www.bjios.sg right away to know more.