Without doubt, running comes with incomparable benefits many people don’t want to miss out on.
However, while highly beneficial, running can also cause injuries that will require a visit to orthopaedic specialists for those who are not careful.
Statistics indicate that at least 80 percent of runners get injured annually.
Most of the injuries runners suffer from can be attributed to training changes, weak hips, and overuse, among other things.
Below are some of the most prevalent running injuries that plague runners, the possible culprits, preventive measures, and the likely treatment options available:
Ankle Sprain
When the ligament is stretched beyond its limit, a sprain occurs.
Oftentimes, ankle sprains occur when the ankle rolls in or outward.
Curbs, tree branches, potholes, and at times, an unfortunate landing can result to ankle sprain.
Recovering from ankle sprain can take some time but performing balance exercises (i.e. single-legged squats) are recommended to help strengthen the muscles while recovering.
Getting ample rest is also highly recommended.
Depending on the condition’s severity, scheduling an appointment with orthopaedic specialists might be required so an effective and more specific treatment plan is created.
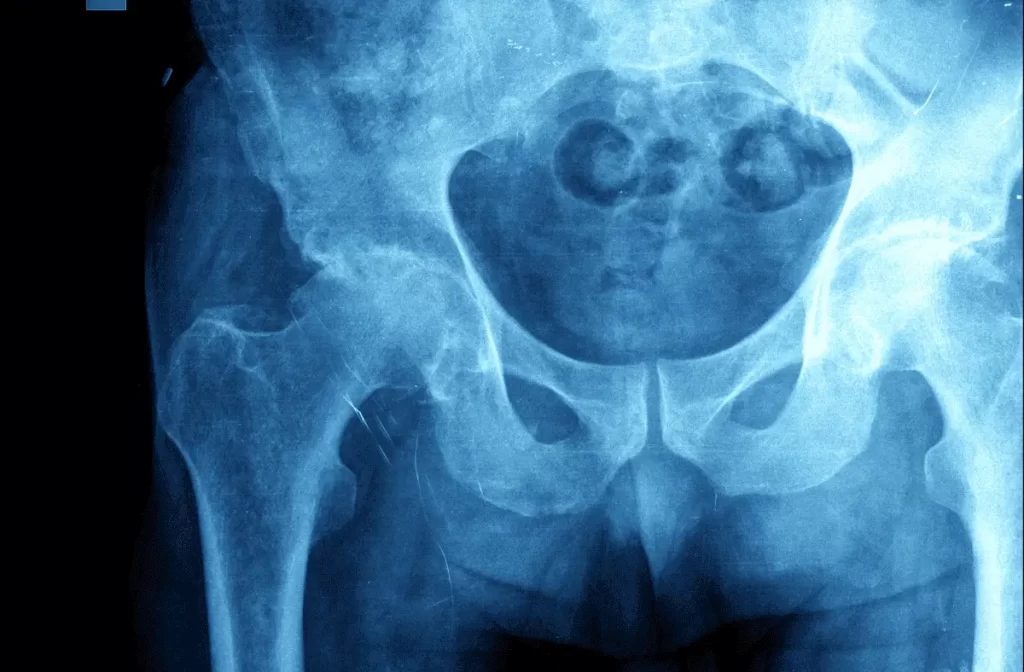
Iliotibial Band Syndrome
Iliotibial band syndrome or ITBS occurs when the Iliotibial band (the thick tendon that stretches from the pelvic bone to the thigh) becomes swollen.
Weak hips, increased mileage, and downhill running are often the likely culprits.
To significantly reduce the pain, it would be a good idea to show the muscles some love.
For starters, do specific stretches and foam rolling to help minimize the pain and the inflammation.

Achilles Tendinitis
Achilles tendinitis occurs when the tissues that connect the heel to the lower leg muscles become swollen.
The condition can be attributed to a lot of factors—naturally flat food, tight calf muscles, improper footwear, drastic mileage increase, to name a few.
To ensure Achilles tendinitis is kept at bay, stretching the calf muscles before and after working out is recommended.
Also, when possible, refrain from doing hill climbs as it can put unwanted strain and stress on the tendons.
Anti-inflammatories, stretching, and the R.I.C.E (rest, ice, compression, and elevation) technique can help affected runners get right back on track in no time.
Patellar Tendinitis
Otherwise known as “jumper’s knee,” patellar tendinitis is very common among distance runners.
Patellar tendinitis occurs when tiny tears in the patellar tendon will manifest as a result of overuse.
Common causes of the condition include overpronation, too many hill repeats, and over-training.
To help reduce the risk of developing the condition, strengthening the hamstrings and quads is recommended.
To ease the pain, putting ice on the affected knee will help significantly.
To help soothe and strengthen the tendon, physical therapy might be prescribed.
Runner’s Knee
Runner’s knee or patellofemoral pain syndrome is often characterized by tender pain around or behind the knee cap.
Runner’s knee can be attributed to several factors including downhill running, weak hips, muscle imbalance, and repetitive pavement pounds during runs.
In order to avoid runner’s knee, running only on flat or soft surfaces is recommended.
However, for those who already have runner’s knee, taping or bracing the knee might be prescribed.
Taking anti-inflammatory drugs or reducing your mileage are other options you can look into.
Shin Splints
For those who have been running for quite some time, they have likely encountered shin splints at one point or another.
Often characterized by aching and stabbing sensation, the condition occurs when the muscles and tendons covering the shinbone becomes swollen.
Icing the affected area (for at least 15 to 20 minutes) has been proven to help reduce both the swelling and the pain.
Elevating the leg affected may also help.
Prevention of shin splints is considered tricky, but researchers discovered that shock-absorbing insoles can help as it can provide the support to the arch.
Keep running injuries at bay and effectively manage any running injuries you have by heading to www.bjios.sg now!











 .
.




