Many years ago, joint replacement surgery was deemed a high-tech procedure.
Nowadays however, it’s already considered ordinary.
In fact, on a yearly basis, surgeons replace more than a million hips and knees.
And that statistics is in the United States alone.
The staggering number of joint replacement surgery performed is actually not surprising taking into account the benefits (improved mobility and significant pain relief) hip and knee replacement surgeries offer.
For the right patients, hip and knee replacement can be a highly beneficial and life-changing procedure.
Hip Replacement
The procedure carried out to remove the hip joint’s damaged parts is called hip replacement.
Those with ankylosing spondylitis, rheumatoid arthritis, and severe osteoarthritis are some of the possible candidates for hip replacement surgery.
Patients suffering from hip fractures secondary to osteoporosis are also likely candidates. In majority of the cases however, the procedure is performed to remedy joint damage.
The extent of hip replacement will depend on the severity of the joint damage.
Akin to knee replacement, the procedure is only resorted to when all other conventional and nonsurgical treatments have offered little to no relief.
Otherwise referred to as hip arthroplasty, hip replacement surgery becomes the likely resort when the pain becomes too severe and starts interfering with the patient’s typical day-to-day routines.
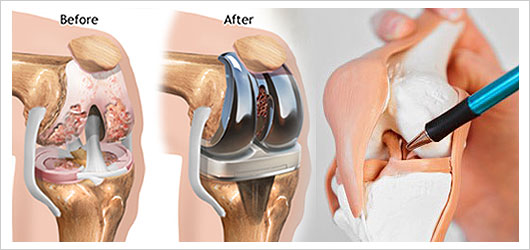
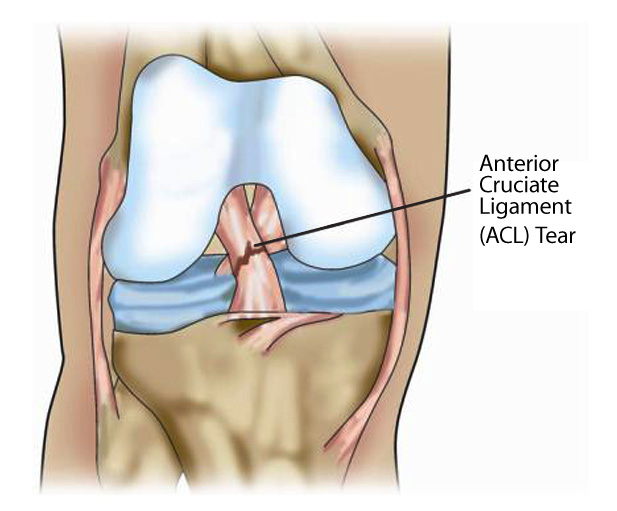
Knee Replacement

Individuals suffering from osteoarthritis are often the likely candidates for knee replacement surgery.
Oftentimes, the knee is the most affected body part as it bears the body’s weight.
Just like hip replacement surgery, the procedure is only performed when all other conservative treatment options have failed.
Just like other surgeries, knee replacement also comes with certain risks.
Some of the common risks include:
- Infection
- Heart attacks
- Stroke
- Blood clots (in the leg veins or lungs)
- Nerve damage
Knee replacement surgeries are often performed by orthopedic surgeons.
Before the surgery, the knee’s strength, range of motion, and stability will be assessed.
If you are a candidate for joint replacement, below are some of the questions you need to ask:
Is it possible for other treatment alternatives to work?
While deemed safe, it would be best to remember that the procedure will still come with certain risks just like any other surgery.
Recovery period can also take several months.
Taking that into account, make sure all other treatment alternatives have been explored before deciding on joint replacement procedure.
Has the procedure been discussed thoroughly by the doctor?
If there are questions about the procedure that you need enlightenment on, it would be best to list them down and ask your doctor to provide insights and enlightenment.
If there are certain doubts that you need discussed, you can get peace of mind by asking your doctor about it.
Also, it is recommended that you ask what the procedure would be like and what you can expect while recuperating.
Have I taken time out to research about the procedure?
Apart from the information your doctor or surgeon will provide, it would be wise to also do your own research so you’ll have all the bases covered and you’ll know the ins and outs of what you will be getting yourself into.
Look for reliable websites so you are sure you are sure the information you will be getting is as accurate as possible.
Better yet, it would be best to visit www.bjios.sg to check the best treatment route for your case.