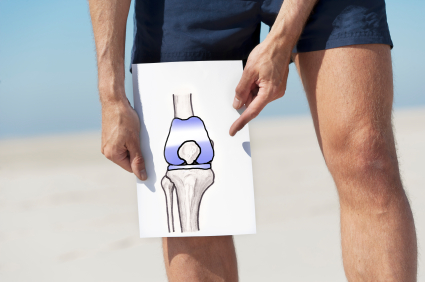
Years prior, joint replacement surgery was considered a high-tech procedure.
Nowadays, it is already considered a common operation.
In fact, in the US alone, statistic indicate that more than a million hips and knees have been replaced yearly.
While the figure is relatively high, it is actually not surprising.
Given the procedure is right for you, hip and knee replacement can be truly life-changing.
Statistics show that a staggering 90 percent of individuals who have had joint replacement surgery notice a dramatic change in terms of mobility and pain relief.
When is hip and knee replacement truly required?

There are several key factors surgeons take into consideration to determine candidates for joint replacement surgery.
Some of the factors include:
Pain and stiffness – joint replacement is considered a likely option for those who experience excruciating pain and are no longer able to carry out routine activities like walking, getting up from a chair, or climbing the stairs, among others.
Deformity – joint replacement surgery is a probability when the affected leg becomes severely swollen or bowed.
Bone damage – when there is severe joint damage due to osteoarthritis and other conditions, joint replacement might be required.
Poor life quality – aside from the pain, surgeons would need to consider if the joint issue has already affected the patient’s quality of life. If it already limits the patient’s movements or causes them to be depressed or grumpy, then joint replacement might be necessary.
Even in cases where all of the requirements for joint replacement surgery has been met, certain factors still need to be taken into consideration to truly gauge if the procedure is indeed the right option.
Ask yourself the following questions to help accurately gauge if you have made the right decision:
Am I willing to make the necessary adjustments/changes?
Achieving the optimum results entails dedication to making the right changes. In other words, you need to become disciplined in terms of losing any excess weight, exercising more, eating healthier, and adapting a healthier lifestyle in general.
Do I have someone to help me out while I’m recovering?
Recovering from joint surgery without help would be extra challenging, if not totally impossible.
For starters, you would need assistance doing just the basics alone—moving around, getting dressed, preparing food, changing the bandages, among other things—especially during the first few weeks.
If you don’t have family members or close friends helping you out, consider checking for rehab facilities you can check in at least while you are recovering.
Have I tried all the other conventional options?
While deemed safe and effective, there are still certain risks involved in joint replacement injuries, much like any other surgeries.
In addition, recovery time can definitely take a lot of months.
Ideally, it would be best to exhaust all other conventional and noninvasive options before considering surgery.
While no doubt life-changing, joint replacement surgery might not be the ideal treatment recourse in all scenarios.
For instance, the procedure is not exactly a good alternative given the following scenarios:
Infection – if patient has suffered from a recent body infection, joint replacement is not a viable option. Understandably, caution should be exercised in order to prevent the infection from spreading to the joint area after the surgery. In cases where the infection spreads, it might result to more serious concerns and might even require additional surgery.
Pain cause – surgeons will have to make sure the pain is really secondary to joint damage and not anything else. Bear in mind that there are hip and knee issues that joint replacement surgery will not fix.
Other medical issues – if patient has a history of uncontrolled diabetes, strokes, or heart attacks, complication risk becomes relatively higher.
Hip and knee replacement is not for everyone. To know if it is the best treatment intervention for your case, visit www.bjios.sg now.